US Heart Health Statistics Bring Sobering News
American hearts are in trouble with the pandemic and a resurgence of smoking among some groups to blame.
Newly released statistics from the American Heart Association and the National Institutes of Health paint a sobering picture of America’s heart health. This is especially prevalent among minorities, including those of African, Caribbean, Asian and Hispanic descent.
Recent Threats
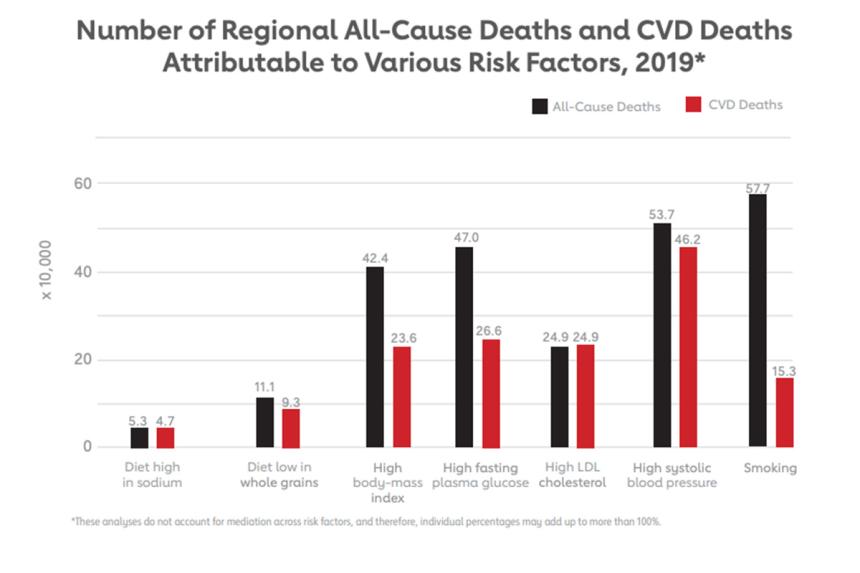
Every year the AHA and NIH publish statistics on a range of heart diseases, circulatory conditions, stroke and their associated risk factors. The association and the institute track stats to understand how heart disease and its contributing elements evolve and how to tackle the public health challenge. Heart disease is the leading cause of death in the U.S.
This year, however, AHA included additional data on COVID-19. Although COVID-19 is a respiratory virus, it’s known to affect and even cause permanent damage to the cardiovascular system. While COVID-19 lowered the overall life expectancy of Americans, it took a particularly harsh toll on some ethnic groups, leading AHA to focus some of the data collection on how COVID-19 affected American minorities.
Why was this past year rougher than usual? There were two standout factors: tobacco use and COVID-19 associated heart damage, according to the report published in the journal Circulation.
Tobacco Use
Smoking is the leading cause of preventable disease, death, and disability in the U.S., according to the U.S. Centers for Disease Control and Prevention. Fortunately, smoking in the U.S. declined from almost 21 percent of American adults to almost 13 percent between 2005 and 2020. However, despite the drop, the AHA report found members of marginalized communities such as indigenous populations like American Indian/Alaskan Native and LGBTQA have much higher smoking rates compared to the general American population.
Smoking is dangerous because the chemicals in cigarette smoke inflame the cells that line blood vessels. This causes blood vessels to narrow, raising the risk for conditions such as:
- Atherosclerosis
- Coronary artery disease
- Stroke
- Peripheral artery disease
- Abdominal aortic aneurysm
This led manufacturers to develop electronic cigarettes. Vaping gained traction over the last couple of decades as potentially healthier – possibly even lifesaving -- alternative to smoking combustible cigarettes.
AHA’s update found that a higher percentage of teens use e-cigarettes than adults. A University of Pennsylvania study concurred with AHA’s results that many teens are vaping. In fact, they estimate that half of all high school students have tried it at least once and about one-third became regular users.
However, e-cigarettes are not a healthy alternative to combustible cigarettes. They’ve been found to be addictive and contain dangerous chemicals. Studies suggest vaping can lead to progressive lung disease and impair blood vessels, raising the risk for heart disease.
“If you or a loved one smokes or vapes, quitting can be lifesaving. Over time, your cardiopulmonary system heals,” says Bernard Kaminetsky, MD, medical director, MDVIP. “Studies have found that within five years of quitting combustible cigarettes, smokers lower their risk of stroke to about that of a person who has never smoked.”
Covid-19 Related Heart Damage
By July 2022, more than 1,000,000 COVID-19 deaths had been reported in the U.S. Unfortunately, many survivors had significant residual health issues, such as heart damage. The risk of heart problems one year after a COVID-19 infection was substantial, according to a study published in Nature Medicine. Heart problems can be divided into three categories:
The AHA report also identified three pandemic related risk factors that raised the risk for permanent heart disease conditions.
- Lack of physical activity – most gyms, recreational centers and studios closed during the pandemic, leaving people with a limited ability to workout. Staying home also curbed daily physical activity routines like walking to and from work parking lots, around the mall or in downtown areas over weekends. AHA found that being sedentary significantly raised the risk for a COVID-related hospitalization or death.
- Skipping doctor visits – many people chose to stay home during the pandemic, skipping doctor visits that monitor heart disease and its risk factors like high blood pressure and high cholesterol. The AHA report indicated weekly cholesterol testing rates declined by more than 39 percent in 2020.
- Reluctance to seek medical care – many people either chose not to seek medical care or were unable to seek help during the pandemic. This caused a greater demand for acute and urgent healthcare needs for issues that could have been managed as a chronic condition.
Other studies also point to Americans gaining a lot of weight during the pandemic. Obesity contributes to heart conditions by raising your risk for irregular heartbeat, heart failure and coronary artery disease.
“The take home message from this report is that many Americans continue struggling with post-pandemic heart issues, especially those who fall into marginalized communities,” says Kaminetsky. “I can’t emphasize enough the importance of working with your primary care physician to help mitigate heart health issues and risk factors that developed during the pandemic.”
Looking for a primary care physician? Consider partnering with an MDVIP-affiliated physician. Physicians in MDVIP-affiliated practices can customize a wellness plan for you that includes helping prevent and control high blood pressure. Find an MDVIP affiliate near you and begin your partnership in health »


