Focus Less on Your Cholesterol Screening and More on These 3 Tests
I realize it’s already February, but I have a resolution for you. Focus less on your cholesterol numbers. Make 2018 the year you switched your attention to your insulin level, inflammation level and LDL (bad cholesterol) particle number.
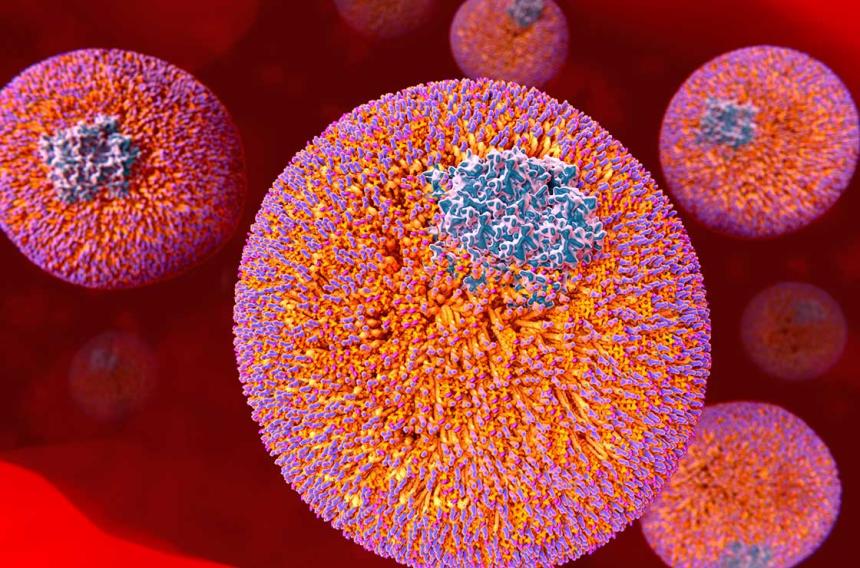
Yes, I know, for years you’ve been told that cholesterol screenings are imperative because elevated LDLs damage blood vessels and raise your risk for cardiovascular disease, heart attacks and strokes. Over the years, low-density lipoprotein became such a concern that ordering a cholesterol profile (total cholesterol, HDL, LDL) and triglyceride screening became routine and considered the gold standard in lab work. But it shouldn’t be.
Why do I believe this? It’s because fifty percent of heart attacks occur in people with perfect cholesterol. This statistic implies that other variables must be involved.
If your doctor is still relying only on cholesterol lab work to base your risk for heart disease, they might be missing the boat. For more information on cholesterol, read my blog, Are You in Your Doctor’s Blind Spot >>
Instead of just ordering a cholesterol profile (total cholesterol, HDL, LDL) or triglyceride screening for a patient, I also order these three tests.
Fasting insulin: Controlling your insulin levels should be your doctor’s first and foremost priority, making a fasting insulin test a necessity. Your results should be 5 or under, although between 5 and 9 is acceptable.
Controlling your insulin level isn’t always easy but it’s possible. In fact, ALL my 90-year-old patients have low insulin levels.
What works? Regular exercise is key, particularly strength training and moderate aerobic training like walking. A low-carb, high-fat diet is essential. Berberine, a chemical extracted from plants and sold in supplement form can help. And of course, the prescription medication metformin.
Inflammation marker(s): How inflamed are your arteries? The level of inflammation in your body helps predict your short-term risk for a cardiac incidence. Many different types of inflammation markers exist but most traditional medical practices use:
- hsCRP: to measure C-reactive protein which is produced in the liver when inflammation is present.
- GGT: to measure gamma-glutamyl transferase, an indicator of liver dysfunction.
- Ferritin: to measure serum ferritin. It’s not clear if elevated serum ferritin causes inflammation or is the result of it.
However, in my practice, we use several types of inflammation markers, but the two tests I rely most heavily on are:
- Lp-PLA2: to measure lipoprotein-associated phospholipase A2, an enzyme that seems to play a role in inflammation and promote atherosclerosis.
- MPO: to measure myeloperoxidase, an enzyme that’s released when blood vessels are inflamed.
LDL particle number: Don’t confuse an LDL particle test with an LDL cholesterol screening – there’s a big difference. An LDL particle test determines the number of LDL particles you have and evaluates them for size, density and electrical charge; whereas, an LDL measurement in a cholesterol screening is more about the ratio of LDLs compared to high-density lipoproteins (HDL), triglycerides and total cholesterol.
Your LDL cholesterol can appear perfect in a cholesterol screening but have a dangerously high number or size of particles, triggering plaque development. LDL particle test reveals your longer-term risk.
If your fasting insulin test, inflammation marker test and/or LDL particle test render abnormal results and you (and maybe your doctor) are unsure not sure of the next appropriate step, consider a coronary calcium score. This CT scan of your heart takes pictures of arteries to verify the amount of arterial plaque. It’s the gold standard for predicting 10-year cardiac mortality and overall mortality. If you score 0, your arteries have no visible plaque and you pretty much have a “get out of heart attack card” for 10 years!
Consult your primary care physician about arterial tests. And if you liked this blog post, you can follow Dr. Malinow on his Facebook page – www.facebook.com/LouisMalinowMD. Are you interested in an MDVIP-affiliated physician? Find one near you and begin your partnership in health »
This blog reflects the medical opinion of Dr. Lou Malinow, an MDVIP-affiliated internist, board-certified hypertension specialist and Diplomate of the American Board of Lipidology, and not necessarily the opinion of all physicians in the MDVIP national network.


