Popular Body Fat Measurement Is Flawed
It’s not news that a high percentage of body fat raises your risk for heart disease, type 2 diabetes and some types of cancer. That’s why it’s a good idea to keep tabs on your body fat percentage.
But the most common measure used by physicians is flawed, according to a new policy adopted by the American Medical Association.
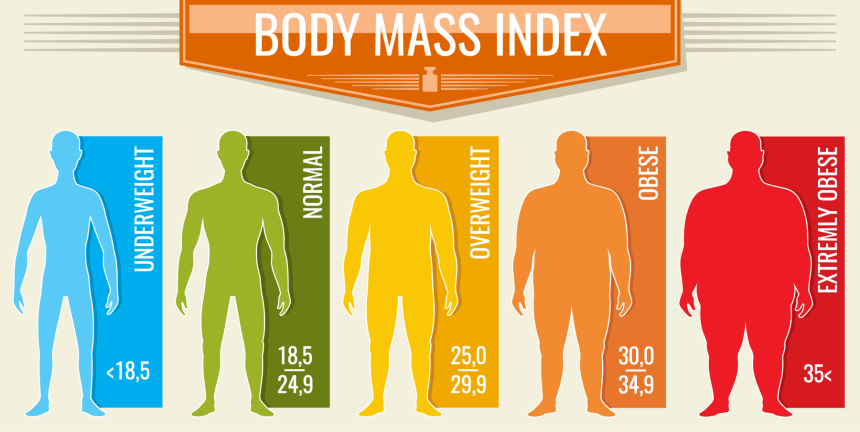
Called body mass index or BMI, this measure has been used for years as a indicator of risk for many kinds of diseases. Despite its popularity, the screening is flawed, the AMA says. Here’s why:
- BMI Is only based on height and weight. It doesn’t account for other components of your body’s composition such as bones, water, organs or muscle.
- The measure can’t determine if weight is muscle or fat. This is important, as muscle is much denser than fat and appears very differently on a body. For example, if you gain 20 pounds of fat, you may look chubbier and not to fit into your clothes; while an additional 20 pounds of muscle can make you look a lot more fit.
- BMI can’t determine if you’re skinny fat. This is when you’re your body fat percentage weight is high, but your weight is low enough to score well on the BMI.
- The methodology is based on data collected between the 1960s and 1990s from White Americans. This means its value is limited for Americans of other ethnic and racial backgrounds.
- It can’t differentiate between genders. Males naturally have more lean mass than women, and both genders accumulate fat mass differently.
- BMI can’t capture age-related loss of muscle mass, function and strength.
“BMI has its place. If you’re overweight and not working out, it can help you, your doctor, personal trainer and/or dietician set some basic goals. And it’s an efficient tool for researchers to recruit and track study participants,” says Bernard Kaminetsky, MD, medical director, MDVIP. “But it probably should not be used as stand-alone metric to determine obesity. That’s one of the reasons most MDVIP-affiliated doctors use body composition scales in the MDVIP Wellness Program. They give us a more nuanced look at muscle and fat percentages.”
In June 2023, the AMA adopted a new policy to clarify the role of BMI screening in medicine. AMA believes the BMI shouldn’t be used as a sole method of diagnosing weight issues.
But BMI accuracy isn’t the only problem. It also doesn’t have a strong link to mortality as other methods of body composition do, including skinfolds, girth measurements, hip-to-waist ratio and bioelectrical impedance analysis. In fact, researchers found the association between BMI and mortality to be inconsistent, particularly for overweight people, according to a study published in PLOS ONE.
Researchers from Rutgers Robert Wood Johnson Medical School analyzed survey data collected between 1999 and 2018 to pinpoint BMI trends. They found an association between BMI-identified obesity and an increased risk of death from all causes. Researchers didn’t look specifically at heart disease or type 2 diabetes, which is important to note as those two conditions, along with high blood pressure, are among the leading causes of premature death in the U.S. and an elevated BMI contributes to these diseases. Researchers did, however, examine BMI-identified overweight and BMI-identified healthy weight and didn’t find a bearing on mortality, suggesting BMI has limited value.
A previous study conducted by the same research team yielded similar results. Researchers tapped 554,000 multiracial and multiethnic U.S. residing participants of the National Health Interview Survey. They conducted a BMI and analyzed self-reported data on men and women with an average age of 46. Researchers followed up with study participants about nine years later and found the mortality risk rose for adults whose BMI fell into the obese and underweight categories.
Adults in the healthy weight and overweight categories had about equal mortality rate, which contradicts existing research. Interestingly, results showed that once Latinos reached a BMI of 27 or 28 (overweight), their mortality risks began rising. Researchers considered this logical as many Latinos tend to develop central obesity (abdominal fat), which has ties to a higher rates of all-cause mortality risk.
“Both of these studies have some limitations, such as using self-reported data. However, the researchers did a great job highlighting the most important drawback of BMI – inaccurate assessment of mortality risk,” says Kaminetsky. “MDVIP has always been ahead of curve when it comes to body composition. The annual wellness program includes bioelectronic impedance, a scale that flows a weak electric current through the body so that voltage can estimate body fat, muscle mass and water weight, and provides a lot more information than BMI.”
If you don’t have a primary care physician, consider partnering with an MDVIP-affiliated physician. MDVIP doctors have the time to work with you and develop a wellness plan that can help you manage your body composition. Find a physician near you and begin your partnership in health »


